When you decide the time is right to become parents, there’s a general timeline most experts note. If you’re under 35 and healthy, you can reasonably expect to become pregnant within a year of actively trying. If you’re healthy and over 35, experts recommend trying for six months before consulting with a fertility specialist about possible pitfalls. In either case, you’re looking at six to twelve months of preparation for a potential pregnancy. So, what can you expect before you’re expecting? This preconception window should be a time to prioritize your fertility health for the best chance of a healthy conception, pregnancy and baby. Here’s what that means, and how to do it.
Key Takeaways
- The preconception window is an important time to prepare the body for what’s to come.
- The preconception health of both parents has a direct impact on conception and the health of your pregnancy and baby.
- Couples should take steps to prepare their bodies for conception by taking prenatal vitamins, embracing a healthy lifestyle and finding healthy ways to manage stress.
What Is Preconception Health?
The preconception window is the period of time roughly three to six months before you become pregnant. Preconception health is the health of men and women during this stage. It’s technically defined as the medical, behavioral and social health of parents-to-be during these reproductive years, which means it may look a little different for everyone. Some couples may need to prioritize stress management, for example, while others focus on better nutrition habits. Regardless of where your preconception health is currently, taking steps to be as healthy as you can during this timeframe is incredibly important.
Research shows that the health of both parents-to-be during this window not only affects conception, it also influences the health of the pregnancy, the baby and the next generation (1). Clearly, there’s a lot at stake, and the more you understand about what can be done during this critical stage, the better!
Preparing Your Body For Conception
While you may think that tossing your prenatal vitamins and hopping into bed covers all your let’s-get-pregnant bases, there’s a lot more you can—and should—do when you want to become a parent. Let’s take it step by step.
Start taking prenatal vitamins
This is one of the simplest and most meaningful ways to support your fertility health in preparation for pregnancy. Experts recommend that both partners begin taking high-quality prenatal vitamins at least three months before conception to ensure a consistent stream of key micronutrients that support both male and female reproductive processes. That timeline is significant, despite the differences in male and reproductive cycles, and worthy of a little discussion.
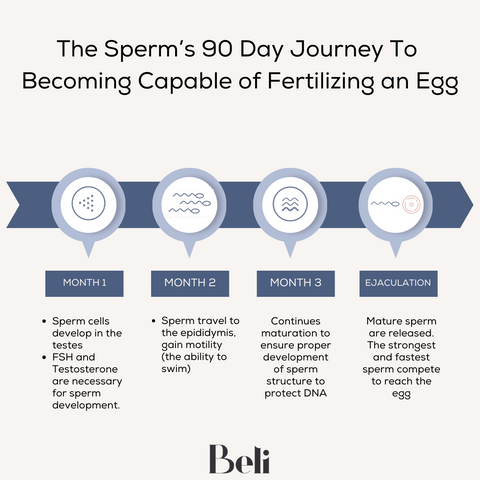
The three-month cycle in men
Men produce millions of new sperm every day, but there’s a lot of maturing that needs to happen before those little swimmers are ready for prime time.
- Phase one: Diploid sperm cells divide into haploid spermatids carrying genetic material
- Phase two: Hormones help spermatids mature into spermatozoa in the testicles, where they’ll remain until they’re almost fully material. During this time, sperm cells will develop a head filled with genetic material and a long tail.
- Phase three: Mature sperm move to the epididymis, a kind of storage tube that preserves sperm in anticipation of ejaculation. Here, sperm become mobile.
A prenatal vitamin like Beli Vitality for Men nourishes sperm health throughout this process. Taking a daily prenatal vitamin helps ensure that maturing sperm have the specialized nutrition necessary for optimal sperm health, and science shows that specific nutrients during this timeframe are linked to sperm production, quality, motility, concentration and DNA quality (2)!
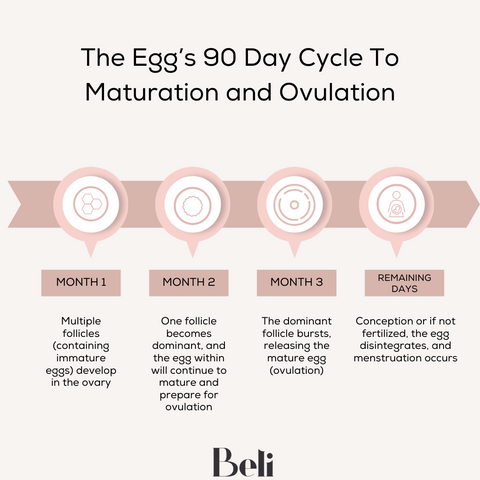
The three-month cycle in women
Women don’t produce new eggs the way men produce new sperm, but human eggs still go through a complex growth process in preparation for fertilization. Notably, the maturation process from oocyte (immature egg) to an egg ripe for ovulation is around three months, and again, this is a prime opportunity to nourish egg quality! Dormant oocytes are located in the ovaries until they begin developing in a follicle (situated in the outer layer of the ovaries). Each cycle, follicles begin this development process and in most cases, a single egg will fully mature and be released from its follicle during ovulation.
Beli for Women is designed to deliver key nutrients during this three-month time frame to support egg quality and balance hormones. Should you conceive more quickly than anticipated, your baby will be getting choline and folate, both of which are instrumental for preventing major birth defects.
A word on birth control and prenatal vitamins
For women coming off birth control, there’s another benefit to your prenatal vitamin. A little-known side effect of hormonal birth control is nutrient depletion, and specifically, vitamins B6 and B12, folic acid, magnesium, vitamin C and zinc. It’s subtle, but it also builds with time. That means the longer you’re on hormonal birth control, the more the decline can add up. Many experts recommend taking prenatal vitamins and hormonal birth control concurrently, to minimize this decline, but certainly after you’ve come off birth control in anticipation of pregnancy.
And while we’re on the topic: Don’t fall for the gimmicky marketing messages that you need to “cleanse” after coming off birth control. There is no scientific evidence that this is the case, and hormonal forms of birth control don’t build up in the body and wreak havoc on your fertility. The focus is simply on rebuilding nutrient stores.
Tune into your cycle
If you aren’t already paying close attention to your period, and especially if you’re coming off birth control that artificially managed your cycle, now is the time. While you may conflate your period with your cycle, there’s a lot happening under the radar!
Your menstrual cycle is divided into phases:
- Follicular: This phase begins on day one of your period, during which the brain prompts the release of follicle-stimulating hormone (FSH), triggering the development of a follicle containing one egg, as we covered above. As the follicle matures, estrogen is released to stimulate the growth and thickening of the uterine lining.
- Ovulation: Phase two begins roughly 16 days after day one of your period, when the ovary releases the mature egg into the fallopian tube. Ovulation is the shortest phase of the menstrual cycle, about 24 hours long.
- Luteal: Phase three begins when the ovary releases progesterone to further prepare the uterine lining for the possibility of embryo attachment. If no conception occurs, progesterone levels drop and your period begins. This phase is typically 12 to 14 days long.
Use an app or track things the old-fashioned way in a day planner, making note of the first day of your period and how long it lasted so you can get an idea of your cycle duration. That way, you can get a rough idea of when you’re ovulating—and the best time to have sex.
Embrace a healthy lifestyle
This is the boring stuff, the low-hanging fruit, the things you know you should but don’t always feel like doing it. We’re talking about getting regular exercise, getting enough sleep, drinking enough water, eating a balanced diet with lots of healthy fats and protein and veggies, and taking care of your mental health, too (3)(4)(5). In short, anything that supports and improves your overall health has a trickle-down effect on your reproductive health. Plus, you might find the idea of parenthood makes you feel more motivated to embrace these healthy habits.
Talk to your doctor
Before trying to conceive, it can be really helpful to see your doctor for a discussion on preconception health. It’s an opportunity to discuss your health history and any medical issues that might affect a pregnancy, including PCOS. Make a point of sharing any current medications as well, and you might even consider getting your nutrient levels tested to ensure you’re getting enough vitamin D. Most people aren’t!
Consider an at-home sperm test
Women may be able to chat up their gynecologist when they’re ready to become mothers, but men don’t often have the cozy relationship with a reproductive specialist. That’s where an at-home sperm test can prove useful. While the information is limited—you can generally expect details relating to sperm volume, concentration and motility—it serves as a baseline picture of your current sperm health. And that can be pretty illuminating.
The Bottom Line

So, what should you expect before you’re actually expecting? Ideally, doing everything you can to put your fertility health first. The truth is, so much of the pregnancy equation is beyond our control. But the lifestyle factors and choices and habits that we can influence can have an enormous impact, so it’s absolutely worth putting your energy and focus there.
Article Sources
1. Preconception Health. The Lancet. (2018). https://www.thelancet.com/series/preconception-health
2. Skoracka, K et al. (2020). Diet and nutritional factors in male (in)fertility—underestimated factors. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7291266/
3. Planning for Pregnancy. (2023). https://www.cdc.gov/preconception/planning.html
4. Panth, N et al. (2018). The influence of diet on fertility and the implications for public health nutrition in the United States. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6079277/
5. Rooney, K et al. (2022). The relationship between stress and infertility. https://www.tandfonline.com/doi/full/10.31887/DCNS.2018.20.1/klrooney



